
10 Awards Reviews What is this? Just a plastic bag?! "It is a Tse mask!" Charles Brandwein, MD, 2001 "It is Totally Simple and Easy!" Jacqueline Gladdis, R.N., 2006 "So Easy! Anesthesiologists can do it!!" James Tse, PhD, MD "Why don't you call it 'TSE-Alloteh CPAP'?" John Denny, MD, 2013 "Nasal Tse-PAP Mask Assembly" Jack (John A.) Pacey, MD, FRCSc, GlideScope Inventor, 2015 Gliscopejack: Near Perfection in Airway Management is Now Possible..Modified Pediatric Nasal Mask, Feb 19, 2018 |
INTRODUCTION The demand for off-site anesthesia care has been increasing in the recent years at the Robert Wood Johnson University Hospital in New Brunswick, NJ. The off-sites include Endoscopy/Bronchoscopy Suite, Cardiac Echo Lab, Cardiac Cath Lab, Radiology/Special Procedure Suite, CT- Scan/MRI Suite, Infertility Clinic, ER and ICUs. These off-sites pose many challenges for anesthesia care providers, such as less-than-ideal anesthesia set-ups, small crowded and dark rooms, help from another anesthesiologist is far away, production pressure for rapid turnover, high expectation, high-risk patients, etc. It is especially challenging during EGD, EUS, ERCP, PEG, bronchoscopy and TEE. An O2 reservoir is lost when the patient’s mouth is kept open with a bite block (Photo 1). A nasal cannula becomes ineffective and delivers only minimal O2 (<0.30 FiO2). Furthermore, the airway is often compromised by the endoscope. Oxygen desaturation is a common occurrence in patients receiving moderate-to-deep sedation during upper GI endoscopic procedures. According to ASGE Guideline (2012), large series report adverse event rates of 1 in 200 to 1 in 10,000 and mortality rates ranging from none to 1 in 2000. Data collected from the Clinical Outcomes Research Initiative database show a cardiopulmonary event rate of 1 in 170 and a mortality rate of 1 in 10,000 from among 140,000 UGI endoscopic procedures. For more information, please go to ASGE Guideline: Adverse Events of Upper GI Endoscopy, BSG Guidelines in Gastroenterology: Complications of GI Endoscopy and SGNA Risks & Complications We have used a simple plastic sheet to convert an ineffective nasal cannula to a face tent since 2001 (Photo 2-5). It takes 10 seconds to prepare at bedside and provides FiO2 of 0.50-0.70 with the nasal cannula O2 flow rate of 4-5 L/min. It improves patient’s oxygenation, prevents severe desaturation, decreases the need for assisted ventilation and reduces the interruptions of the procedures. How to Make a Tse "Mask" We make a 12" x 12" or larger plastic sheet utilizing any clean, clear plastic bag (nasal cannula bags, specimen bags, face mask bags, breathing circuit bags, etc.) or the clear plastic shield of a fluid-shield surgical mask . After the patient assumes the lateral decubitus, prone or supine position, we put a nasal cannula on the patient and then place a clear plastic sheet over the patient’s head covering the eyes, the nose and the mouth, and secure it with tape. (Photo 2-7) In less than 10 seconds, a nasal cannula is converted into a face tent that provides FiO2 of 0.50-0.70 with O2 flows of 4-5 L/min. Upper GI Endoscopy, FOB or TEE During manipulation of the endoscope, we lift the plastic sheet slightly to avoid dragging it into the mouth. The zip-lock specimen and face mask bags are easy to use because the rigid edges can stand up like a tent with an open door (Photo 2-4) The soft plastic sheet can also be re-enforced with one- inch silk tape. (Photo 5) When we use a plastic shield from a fluid-shield surgical mask, we tape the plastic sharp edges to avoid corneal abrasion. (Photo 6) After explaining to the patient that by applying this plastic sheet we will be increasing O2 supply and ask the patient to close the eyes, even the most anxious patients are receptive. Following pre-oxygenation using this technique for 1-2 minutes, we titrate propofol or other sedatives to achieve moderate-to-deep sedation while maintaining spontaneous respirations. Keep a Patent Airway and Monitor Respiration We position patient’s head and neck to maintain a patent airway. For patients with upper airway obstruction, serial dilation with well-lubricated nasopharyngeal airways may avoid causing nasal bleeding. We monitor the patient’s respirations using capnography, with or without a pediatric precordial stethoscope placed over the trachea. This face tent also improves CO2 sampling and makes early detection of respiratory depression possible. If the patient becomes apneic because of airway obstruction or over-sedation, we have an average of 2-3 minutes to manipulate the airway and/or to decrease the level of sedation before desaturation occurs. Rebreathing of CO2? One concern is that a plastic sheet could increase "dead space" resulting in re-breathing of CO2 and hypercarbia. We routinely monitor CO2 using capnography. By maintaining the plastic sheet in a tent-like position with an open door, we can avoid re- breathing of CO2 (Photo 7). Monitored Anesthesia Care The line between deep sedation and total intravenous anesthesia is very fine. Deep sedation often turns into general anesthesia. Anesthesia providers should always be ready to manage patients under general anesthesia. If a nasal cannula is used for deep sedation, a TSE "Mask" will improve patient’s oxygenation. We have used this face tent for short procedures (D & C, hysteroscopy, LEEP,cystoscopy). Precautions If opioid analgesic is needed, titrating in small increments of analgesic would maintain spontaneous respiration. Patient selection is important to decrease the risk of pulmonary aspiration. Premedication of the patient with metoclopramide may decrease the risk of gastric reflux. Nasal Tse-PAP Mask/Circuit Assembly to deliver CPAP, BiPAP, CF (continuous flow) or Assisted Nasal Ventilation for Patients with or without OSA under MAC (EGD, colonoscopy, bronchoscopy, TEE, etc.), Awake Intubation or GA. (Provisional Patent filed on Oct 30, 2013 and Formal Patent Application filed on Oct 29, 2014 by Rutgers University for a similar assembly. James Tse and co-inventors have transferred the invention to RU for one dollar.) (Please see updated Practice Guidelines for Perioperative Management of Patients with Obstructive Sleep Apnea. Anesth 120: 268-86, 2014 or Google search "2014 ASA Guidelines OSA" for a pdf link) Patients under monitored anesthesia care (MAC) receive intravenous sedation and O2 via nasal cannula (NC). Over-sedation and/or airway obstruction may cause severe desaturation, especially in obese patients with OSA. Even with a face tent (TSE "Mask"), obese OSA patients may require frequent chin- lift, jaw-thrust and/or insertion of nasal airways. Inserting nasal airways may cause bleeding despite using small, well lubricated nasal airways. On January 24, 2013, a nasal TSE-PAP mask/circuit was developed using an infant face mask (Photo 11-13). It was successfully used in 3 sedated patients with and without OSA the next day to improve spontaneous ventilation and oxygenation during EGD. The effectiveness of nasal ventilation in anesthetized patients and unconscious apneic adults has been shown by Liang et. al. (Anesthesiology 108: 998-1003, 2008 Anesthesiology 108: 998-1003, 2008) and Jiang et. al. (Anesthesiology 115: 129-35, 2011 Anesthesiology 115: 129-, 2011) The nasal TSE-PAP mask is especially useful for EGD and TEE under MAC. With the bite block in place, CPAP is about 1-2 cm of H2O even with the APL valve completely closed. However, it becomes CF mask with fresh O2 flow of 4-5 L/min. Fresh air can be added to keep FiO2 under 0.8 to avoid causing absorption atelectasis (Photo 11-18). Precautions: Adjust the APL valve to deliver 4-8 cm H2O CPAP as needed and avoid over- inflating the reservoir bag. If the patient becomes apneic or the airway is obstructed by the endoscope, assisted ventilation can be immediately delivered without interrupting the procedure. It should be done with small volume to keep PIP under 20 cm of H2O to avoid gastric insufflation. Should you have any question for the safe use of this technique, please contact us via (contactus) or email (james.tse@rutgers.edu) It improves oxygenation and can be used to pro- actively prevent desaturation in obese patients with OSA. ( Please see Publications #70 & 71, 81-85, 87-95) (Patients consented for photography) This nasal mask assembly has also been used for awake FOB and/or video laryngoscopy assisted endotracheal intubation (Photo 19a-c) and preoxygenation and assisted nasal ventilation for patients with poor face- mask fit during induction of general anesthesia (Photo 19d-g). (Please see Publication and Presentation). A Modified TSE "Mask" for Upper Body Procedures Fire Hazard Precautions Do not use a plastic bag or a plastic sheet for upper body procedures, such as breast biopsy or thyroidectomy to avoid high O2 concentration Pooling under the surgical drapes. Taping a fluid-shield surgical mask firmly to the lower jaws will decrease the risk of FIRE HAZARDS. (Photo 22-24) It increases O2 supply to the patient and avoids O2 pooling under the surgical drapes close to the surgical site. Our preliminary data show that O2 concentration under the surgical drapes is close to 22% by using this modified TSE "Mask". It also keeps the surgical towels or drapes from covering the patient's face. It is very important to protect the eyes. Tape the sharp edges of the plastic shield to avoid corneal abrasion. (Photo 22-24) Even though there are commercially available devices for endoscopies or for patients with mouth breathing (Photo 20-24), this technique utilizes plastic sheets which are ubiquitous and available at no additional cost. We also use this technique for patients undergoing rectal procedures in the jack-knife position (Photo 25), pain management procedures in the prone position, retrobulbar block (Photo 28) and pediatric procedures (endoscopy, PICC, spinal tap, bone marrow biopsy, MRI, CT Scan, etc.). Precautions Prone Position: Use pillows to support the upper body and head to maintain a patent airway. For patients with upper airway obstruction, serial dilation with well-lubricated nasopharyngeal airways and chin lift may open the airway. Use a large clear plastic sheet to create a large O2 hood (Photo 8 & 25). If patient's oxygenation fails to improve, attaching an anesthesia breathing circuit to a nasopharyngeal airway using an ETT connector delivers high concentration of O2 directly into the oropharynx (Photo 26-27): 1. The connector from a 7.0 ETT fits well with 30-34 Fr nasopharyngeal airways (so does a 6.0 or 8.0 ETT connector with 26- 30 Fr and 32-34 Fr nasopharyngeal airways, respectively) (Photo 27). 2. O2 flow is usually set at 4-6 L/min and the circuit pressure relief valve is opened. 3. To avoid trauma to nasopharyngeal tissue, a well- lubricated small nasopharyngeal way (26 or 28 Fr) is gently inserted to make sure there is no resistance in the airway. After replacing it with an appropriate nasopharyngeal airway, the ETT connector is connected to the nasopharyngeal airway and the breathing circuit is then connected to the ETT connector. 4. If the reservoir bag is over- distended, we need to adjust the pop-off valve to ensure that O2 flow is not excessive which may force secretion into the trachea and/or cause tissue injury. 5. The patient may breathe through the breathing circuit if the nasopharyngeal airway is the only patent airway. By adjusting the pressure relief valve, it provides CPAP that may prevent airway from collapsing. 6. If the patient is apneic because of over-sedation, this technique allows low positive pressure ventilation in order to gain time for sedation to wear off or for turning the patient supine to perform assisted ventilation. 7. We are always prepared to ventilate and oxygenate the patient using a bag-mask or ETT if this approach fails to improve oxygenation quickly. Retrobulbar Block (Photo 28- 29): Tape the face tent over the bridge of the nose and lower cheeks for pre-oxygenation, and remove it before sterilization preparation to avoid suffocating the patient (Photo 29)!! Fexible Fibro-optic Bronchoscopy (FOB) Tape the specimen plastic sheet on the forehead and both cheeks. Cut a hole near the nose or the mouth or tear the plastic sheet to middle to allow bronchoscope for oral (Photo 30) or nasal (Photo 31) insertion of bronchoscope. Overlap and tape plastic sheets together to avoid O2 from disappearing. Modified TSE "Mask" to Improve Pre-Oxygenation of Combative Trauma Patients for Emergency Endotracheal Intubation (Photo 32) Since 2006, many anesthesia attendings in the Department of Anesthesiology have contributed their time and their own financial resources to teach the use of these simple techniques at national and international anesthesiology meetings. Our main goals are to improve patient safety and reduce healthcare costs. Special thanks to all the anesthesia attendings (Dept. Anesthesiology & Perioperative Medicine, Rutgers RWJMS(formerly UMDNJ RWJM0S who have supported us with extra time to present our clinical findings as poster presentations and demonstrate this technique as Scientific and Educational Exhibits. Publications/Poster Presentations Education Please see Anesthesia Patient Safety Foundation 5 Reviews (2007-2010, 2013, 2014) and Anesthesiology News Review (2009 & 2016) Reviews |
| Welcome to www.TseMask.com The Simple Combined Nasal Tse-PAP Mask-Face Tent for Reducing Aerosol/Droplet Spread and Providing Continuous Nasal Oxygenation & Additional Provider Protection during MAC, GA induction, Endotracheal Intubation and Extubation & The Original Tse "Mask" (Face Tent) & Nasal Tse-PAP Mask/Circuit Assembly for Improving Oxygenation & Patient Safety |












Photo 1. Upper GI Endoscopy,
FOB or TEE. With the mouth
kept open by a bite-block, a
patient receives only minimal
O2 via a nasal cannula.
Airway obstruction,
respiratory depression or
over-sedation easily leads to
severe O2 desaturation.
FOB or TEE. With the mouth
kept open by a bite-block, a
patient receives only minimal
O2 via a nasal cannula.
Airway obstruction,
respiratory depression or
over-sedation easily leads to
severe O2 desaturation.
Photo 2. Secure the plastic
sheet with taping along the
forehead and the cheek.
Tape the clear plastic sheet
above the eye and make
sure eyes are closed and
protected.
sheet with taping along the
forehead and the cheek.
Tape the clear plastic sheet
above the eye and make
sure eyes are closed and
protected.
Photo 3. Tape along the
lower jaw.
lower jaw.
Photo 5. Double taping the
edge of a soft plastic sheet
to strengthen the face tent
to avoid interfering with the
scope.
edge of a soft plastic sheet
to strengthen the face tent
to avoid interfering with the
scope.
Photo 4. The rigid edges of
a zip-lock bag stand up like
a tent with an open door.
a zip-lock bag stand up like
a tent with an open door.
Photo 7. ERCP in lateral
decubitus position with
pulse oximetry, O2 and ETCO2
tracings.
decubitus position with
pulse oximetry, O2 and ETCO2
tracings.
Photo 8. ERCP in prone
position.
position.
Photo 9. TEE, PEG or FOB in
supine position.
supine position.
Photo 20. With mouth
breathing, a nasal cannula
delivers minimal O2 and
produces a poor ETCO2
tracing.
breathing, a nasal cannula
delivers minimal O2 and
produces a poor ETCO2
tracing.
Photo 21. Lower Body
Procedures, Cardioversion
or AICD testing: Tape the
plastic sheet to the bridge of
the nose and cheeks or tape it
to the forehead to cover eyes,
the nose and the mouth.. Keep
the lower portion open to
avoid re-breathing CO2. Do
not use a soft plastic sheet
to avoid it from collapsing
and being sucked into the
mouth.
Procedures, Cardioversion
or AICD testing: Tape the
plastic sheet to the bridge of
the nose and cheeks or tape it
to the forehead to cover eyes,
the nose and the mouth.. Keep
the lower portion open to
avoid re-breathing CO2. Do
not use a soft plastic sheet
to avoid it from collapsing
and being sucked into the
mouth.
Photo 22. Upper body
procedures: Tape a
fluid-shield surgical mask
firmly to the lower jaw. Tape
the sharp edges of the
plastic shield to AVOID
CORNEAL ABRASION.
procedures: Tape a
fluid-shield surgical mask
firmly to the lower jaw. Tape
the sharp edges of the
plastic shield to AVOID
CORNEAL ABRASION.
Photo 23. This modified TSE
"Mask" for upper body
procedures increases FiO2 ,
prevents O2 pooling under
the surgical drape and
reduces the risk of FIRE
HAZARDS.
"Mask" for upper body
procedures increases FiO2 ,
prevents O2 pooling under
the surgical drape and
reduces the risk of FIRE
HAZARDS.
Photo 28.
Pre-oxygenation for
retrobulbar block.
Pre-oxygenation for
retrobulbar block.

Photo 25. Jack-knife or Prone
Position. Use pillows to support
the upper body and head to
maintain a patent airway. Tape a
large clear plastic sheet like a drape
over the head. Keep the bottom
open to avoid rebreathing CO2.
Position. Use pillows to support
the upper body and head to
maintain a patent airway. Tape a
large clear plastic sheet like a drape
over the head. Keep the bottom
open to avoid rebreathing CO2.


Photo 6. A plastic shield from
a fluid-shield surgical mask.
a fluid-shield surgical mask.
Photo 10. A plastic shield from
a fluid-shield surgical mask.
a fluid-shield surgical mask.


Photo 26. A simple and
quick rescue technique: An
anesthesia breathing circuit
connected to a
nasopharyngeal airway using
an ETT connetor in a
deeply-sedated patient with
upper airway obstruction in
jackknife position.
quick rescue technique: An
anesthesia breathing circuit
connected to a
nasopharyngeal airway using
an ETT connetor in a
deeply-sedated patient with
upper airway obstruction in
jackknife position.
Photo 27. An anesthesia
breathing circuit is
connected to a 30 Fr.
Nasopharyngeal airway
using a 7.0 ETT connector.
breathing circuit is
connected to a 30 Fr.
Nasopharyngeal airway
using a 7.0 ETT connector.

Photo 24. This modified TSE
" Mask" keeps the surgical
drapes from covering the
face and O2 from pooling
under the surgical drapes.
" Mask" keeps the surgical
drapes from covering the
face and O2 from pooling
under the surgical drapes.

Photo 31. FOB nasal
approach
approach

Photo 30. FOB oral
approach
approach


Photo 29. Remove it before eye
sterilization preparation to
AVOID causing SUFFOCATION!
sterilization preparation to
AVOID causing SUFFOCATION!

Photo 32. Secure nasal
cannula with tape, turn O2
flow to 10 L/min and put the
head in a large, clean, clear
plastic bag. Pre-oxygenate
for a few min, RSI of general
anesthesia and remove the
bag before intubation.
cannula with tape, turn O2
flow to 10 L/min and put the
head in a large, clean, clear
plastic bag. Pre-oxygenate
for a few min, RSI of general
anesthesia and remove the
bag before intubation.




Photo 11. How to
assemble a nasal Tse-PAP
mask/circuit:
Inflate the air cushion of
an infant face mask with
about 10 cc of air and
secure a hook ring from a
toddler mask or an adult
face mask with tape.
assemble a nasal Tse-PAP
mask/circuit:
Inflate the air cushion of
an infant face mask with
about 10 cc of air and
secure a hook ring from a
toddler mask or an adult
face mask with tape.
Photo 12. Secure the mask
with head straps to obtain a
good seal and to avoid
compressing the eyes.
Connect it to the adult
anesthesia breathing circuit.
Tape the nasal cannula to
the lower rim of the bite
block for capnography.
with head straps to obtain a
good seal and to avoid
compressing the eyes.
Connect it to the adult
anesthesia breathing circuit.
Tape the nasal cannula to
the lower rim of the bite
block for capnography.
Photo 13. Pad under the
straps to avoid excessive
compression pressure on
the facial nerves. Cover the
mouth with a clear, clean
plastic sheet (Tse "Mask")
to improve the quality of
capnography and reduce
aerosol spread.
straps to avoid excessive
compression pressure on
the facial nerves. Cover the
mouth with a clear, clean
plastic sheet (Tse "Mask")
to improve the quality of
capnography and reduce
aerosol spread.
Photo 14. A patient with OSA
under deep propofol sedation
during EGD.
A nasal TSE-PAP mask is
connected to an adult breathing
circuit and an anesthesia
machine. The pop-off valve is
closed. Fresh O2 flow is set at 6-8
L/min. Fresh air can be added to
keep FiO2 under 0.8.
under deep propofol sedation
during EGD.
A nasal TSE-PAP mask is
connected to an adult breathing
circuit and an anesthesia
machine. The pop-off valve is
closed. Fresh O2 flow is set at 6-8
L/min. Fresh air can be added to
keep FiO2 under 0.8.
Photo 15. The patient is
breathing spontaneously as
indicated by the capnography
obtained with an air sampling
line of a nasal cannula.
breathing spontaneously as
indicated by the capnography
obtained with an air sampling
line of a nasal cannula.


Photo 19. TEE at the
Echocardiology Lab (no
anesthesia machine). A Nasal
TSE-PAP mask connected to a
mask-bag (+ PEEP valve) with
a flexible extension and a wall
O2 outlet (8-10 L/min O2 flow).
Echocardiology Lab (no
anesthesia machine). A Nasal
TSE-PAP mask connected to a
mask-bag (+ PEEP valve) with
a flexible extension and a wall
O2 outlet (8-10 L/min O2 flow).

Photo 16. EGD with
Dilation
Dilation

Photo 17. Nasal TSE-PAP
Mask/Circuit for an OSA
Patient under MAC during
Colonoscopy
Mask/Circuit for an OSA
Patient under MAC during
Colonoscopy

Photo 18. Nasal TSE-PAP
mask/Circuit for an
OSA patient under MAC
during Hysteroscopy and D&C.
mask/Circuit for an
OSA patient under MAC
during Hysteroscopy and D&C.
Videos: How to use Nasal TSE-PAP Mask/Circuit
to improve oxygenation in an OSA patient under
propofol sedation during SVT Ablation in Cath Lab
How to use Nasal TSE-PAP Mask/Circuit to
improve oxygenation in an OSA patient under
remifentanil infusion during Atrial Flutter
Ablation in Cath Lab
improve oxygenation in an OSA patient under
remifentanil infusion during Atrial Flutter
Ablation in Cath Lab
Video: How to Improve Oxygenation using a Tse "Mask" during EGD.


10 Awards including the
2008, 2013, 2015 & 2016
PGA "Best Exhibit for
Clinical Application";
2008, 2013, 2015 & 2016
PGA "Best Exhibit for
Clinical Application";







Photo 19a. Video
Laryngoscopy assisted
endotracheal intubation
Laryngoscopy assisted
endotracheal intubation
Photo 19b. FOB assisted
endotracheal intubation
endotracheal intubation
Photo 19c. Combined video
Laryngoscopy and FOB
assisted endotracheal
intubation
Laryngoscopy and FOB
assisted endotracheal
intubation
Photo 19d. Pre-oxygenation
and assisted nasal
ventilation during induction
of general anesthesia in a
patient with full beard.
and assisted nasal
ventilation during induction
of general anesthesia in a
patient with full beard.
Photo 19e. Pre-oxygenation and
assisted nasal ventilation
during induction of general
anesthesia in an edentulous
patient .
assisted nasal ventilation
during induction of general
anesthesia in an edentulous
patient .
Photo 19f-g. Pre-oxygenation
and assisted nasal
ventilation during induction
of general anesthesia in
obese patients with poor
face-mask fit.
and assisted nasal
ventilation during induction
of general anesthesia in
obese patients with poor
face-mask fit.
2014 3rd Place Award for Scientific/Educational Exhibit at the ASA Annual
Meeting, New Orleans, LA, Oct 2014, (Feb 2015 ASA Newsletter, page 40-41)
& Anesthesia Patient Safety Foundation E.C. Pierce, Jr., MD, Award for "Best
Scientific Exhibit" (APSF Newsletter February 2015, page 48). Reviews
Meeting, New Orleans, LA, Oct 2014, (Feb 2015 ASA Newsletter, page 40-41)
& Anesthesia Patient Safety Foundation E.C. Pierce, Jr., MD, Award for "Best
Scientific Exhibit" (APSF Newsletter February 2015, page 48). Reviews


A Technically Simple and Effective Universal Precaution
in addition to the Recommended PPEs
amid the COVID-19 Pandemic, March 2020 & Beyond
Combining the Nasal Tse-PAP Mask-Face Tent & Suctioning under the Face Tent May
Reduce Aerosol/Droplet Spread and Provide Continuous Nasal Oxygenation & Additional
Protection to Providers during MAC, GA Induction, Video-Laryngoscopic Endotracheal
Intubation and Extubation see Publications #334-340 for 2020 ASA/PGA & 2021 SOCCA/IARS ePosters
in addition to the Recommended PPEs
amid the COVID-19 Pandemic, March 2020 & Beyond
Combining the Nasal Tse-PAP Mask-Face Tent & Suctioning under the Face Tent May
Reduce Aerosol/Droplet Spread and Provide Continuous Nasal Oxygenation & Additional
Protection to Providers during MAC, GA Induction, Video-Laryngoscopic Endotracheal
Intubation and Extubation see Publications #334-340 for 2020 ASA/PGA & 2021 SOCCA/IARS ePosters


Fig. 1. A tear-drop shaped pediatric facemask is
modified to a rounded triangular nasal mask by
squeezing it for 1-2 mins.
modified to a rounded triangular nasal mask by
squeezing it for 1-2 mins.
Fig. 2. An infant mask (left) and the modified infant
mask (right) that fits most adult noses. The air cushion
is injected with 10 cc air.
mask (right) that fits most adult noses. The air cushion
is injected with 10 cc air.
Fig. 3. A large clean specimen bag is taped to the lower
part of the mask and an adult hook-ring is then taped
over the plastic sheet and the mask.
part of the mask and an adult hook-ring is then taped
over the plastic sheet and the mask.

Fig. 4. A nasal mask-face tent connected with a circuit
and a filter is placed over the nose first and then
secured with elastic head-straps to obtain good
nose-mask seal. The head-straps are crossed over each
other to avoid causing eye injury. Fresh O2 flow of 4 L/min
should be adequate for pre-oxygenation in the OR.
and a filter is placed over the nose first and then
secured with elastic head-straps to obtain good
nose-mask seal. The head-straps are crossed over each
other to avoid causing eye injury. Fresh O2 flow of 4 L/min
should be adequate for pre-oxygenation in the OR.
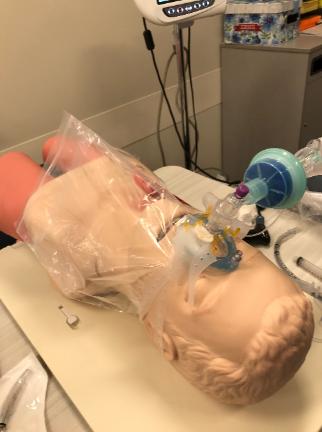
Fig. 5. A patient received pre-oxygenation
with a nasal mask-face tent.
with a nasal mask-face tent.
Fig. 7. If the mouth is open, hold the nasal mask
with the thumb and the index finger and close the
mouth with other fingers over the plastic sheet.
with the thumb and the index finger and close the
mouth with other fingers over the plastic sheet.
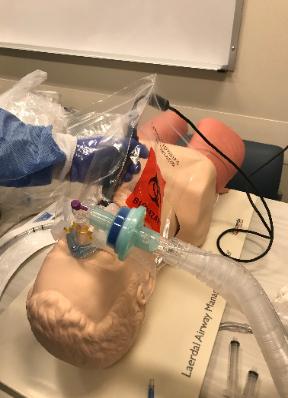
Fig. 9. A disposable video-laryngoscope
(free-standing or hand-held) can be inserted
under the plastic sheet without lifting the cover.
(free-standing or hand-held) can be inserted
under the plastic sheet without lifting the cover.

Fig. 10. Adjust the VL and keep the plastic sheet
cover the mouth.
cover the mouth.
Uses of the Original Tse "Mask" (FaceTent) (since 2001)
and the Nasal Tse-PAP Mask/Circuit (since January 2013)
and the Nasal Tse-PAP Mask/Circuit (since January 2013)

Fig. 11. Keep the plastic cover in place.

Fig. 12. Insert the endotracheal tube under the
plastic sheet.
plastic sheet.

Fig. 14. Inflate the ETT cuff first and disconnect
the breathing circuit and connect it to ETT.
the breathing circuit and connect it to ETT.

Fig. 15. After intubation, check to make sure the
ETT is in the correct place.
ETT is in the correct place.

Fig. 16. Following intubation, oral suctioning
can be done under the mouth cover. Then,
dispose the used plastic sheet properly.
can be done under the mouth cover. Then,
dispose the used plastic sheet properly.

Fig 18. OGT suctioning prior to extubation.

Fig 21. For extubating a patient with nasal tube,
a clean plastic sheet can be used to cover the
nose or the forehead. Following extubation, the
nasal mask with the plastic sheet can be secured
again as described above.
a clean plastic sheet can be used to cover the
nose or the forehead. Following extubation, the
nasal mask with the plastic sheet can be secured
again as described above.

Fig 19.Prior to extubation, the combined nasal
mask and another clean plastic sheet can be
secured over the nose and be ready to use.
Immediately following extubation, check
ventilation through the nasal mask with the
mouth closed as in Fig. 6 and suction the mouth
under the plastic sheet.
mask and another clean plastic sheet can be
secured over the nose and be ready to use.
Immediately following extubation, check
ventilation through the nasal mask with the
mouth closed as in Fig. 6 and suction the mouth
under the plastic sheet.

Fig 20. Immediately following extubation, check
ventilation through the nasal mask with the mouth
closed as in Fig. 6 and suction the mouth under the
plastic sheet.
ventilation through the nasal mask with the mouth
closed as in Fig. 6 and suction the mouth under the
plastic sheet.
Disclaimer: This website is intended for suggestions only and should not be construed as providing
medical advices. The content is not a substitute for the individual practitioner's medical judgment, and
the use of the suggestions portrayed in this website is solely the decision of the individual practitioner.
Dr. James Tse, his colleagues and Rutgers University assume no liabilities for the uses of these
suggestions.
medical advices. The content is not a substitute for the individual practitioner's medical judgment, and
the use of the suggestions portrayed in this website is solely the decision of the individual practitioner.
Dr. James Tse, his colleagues and Rutgers University assume no liabilities for the uses of these
suggestions.

Fig. 17. A clean plastic sheet is taped to the
forehead to cover the nose and the mouth during
EGD.
forehead to cover the nose and the mouth during
EGD.

Fig. 13. Inserting a hand-held VL under the face
tent.
tent.

Fig. 22. Transport a patient to PACU with a face tent
(nasal cannula O2 + a clean plastic sheet covering the
nose and mouth). It traps aerosol/droplet and
increases FiO2 during transport.
(nasal cannula O2 + a clean plastic sheet covering the
nose and mouth). It traps aerosol/droplet and
increases FiO2 during transport.


Fig. 6. A BVM device (Ambu bag) with a flexible
connector and a filter can also be used with wall
O2 supply at the NORA locations. With the PEEP
closed, a low O2 flow (5 L/min) could be used. (A
plastic cover and a filter not shown).
connector and a filter can also be used with wall
O2 supply at the NORA locations. With the PEEP
closed, a low O2 flow (5 L/min) could be used. (A
plastic cover and a filter not shown).


Fig. 8. RSI following pre-oxygenation.
